Highlights
- Small class sizes
- Interprofessional
- State of the art labs
Our Master's in Physician Assistant program will prepare you to provide high-quality health care in a respectful, caring manner.
Are you looking to take the next step in your medical career? Becoming a Physician Assistant is a great option. You’ll have the advanced training to collaborate with one or more physicians and be able to examine, diagnose, treat, and counsel patients. There is a significant need in health care for high-level professionals. At CUAA, we strive to prepare you to provide quality health care in a respectful, caring manner. If you value the same things we do, consider pursuing your Master of Science in Physician Assistant Studies (MSPAS) with us.
We are committed to engaging your mind and spirit for service to Christ in the church and the world.
Our team is available to help you as you consider the next step in your education.
Our team is standing by to assist you with additional program details, financial aid options, and admissions questions.
Loading...
Physician Assistants (PAs) are licensed health care professionals who practice medicine in collaboration with an MD or DO. PAs provide patient care by obtaining histories, performing physical examinations, diagnosing injuries and illnesses, prescribing, assisting in surgery, ordering and interpreting lab and radiologic results and educating patients on their conditions, as well as prevention. PAs work in a variety of settings including hospitals, clinics, universities, governmental services, and industries. PAs are all trained in primary medicine as the basis of their medical knowledge and have the flexibility to practice in any of the different specialties of medicine they desire without having to complete a residency in that field.
There has been, and will continue to be, a significant need in health care for high-level healthcare professionals. Statistics from 2022 by the Bureau of Labor Statistics noted that the median earnings for PAs in 2020 were 121,530/year; with employment projected to grow 31 percent more from 2021 to 2022, which is much faster than the average for all occupations. As demand for healthcare services continues to grow, PAs will be needed to provide care to patients.
In order to become licensed and certified, all PAs must graduate from a PA program that was nationally accredited by the ARC-PA, and pass the Physician Assistant National Certifying Examination (PANCE). Graduates take the PANCE exam after successful completion from an accredited program. Licensure is required in all states.
Licensed and certified PAs are required to complete 100 hours of continuing medical education every two years and pass the Physician Assistant Recertifying Examination (PANRE) every ten years in order to maintain certification.


The PA Program at Concordia University Ann Arbor is intentional in creating an environment of diversity and belonging, welcoming students from diverse backgrounds to become competent medical providers. We welcome and embrace students of any age, race, color, gender, religion, national and ethnic origin, and mental and physical abilities/ disabilities who meet the technical standards. In addition, we are committed to creating a safe and compassionate learning environment for all seeking to improve and influence communities through clinical service and leadership with compassion and respect .
The Vision of the Concordia University Ann Arbor PA Program is to provide the local and global community with competent medical providers who will improve lives and influence communities through clinical service and leadership, and do so in a compassionate and respectful manner that changes the lives of all patients who seek our care.
The Mission of the Concordia University Ann Arbor PA Program is to educate Physician Assistant students in primary medicine with a focus on rural and underserved patient populations and communities.
In meeting our mission, the program has applied for, and been funded, a grant from HRSA to provide student stipends for rural clinical rotations to offset the cost of housing, travel, and food for those students who commit to clinical experiences in rural and underserved areas, in Michigan, as well as any rural and/or underserved areas of the United States.
At CUAA, we strive to prepare you to provide quality health care and to do so in a respectful, caring manner addressing mind, body, and spirit.
If you value the same things we do, consider pursuing your Master of Science in Physician Assistant Studies (MSPAS) with us.
The CUAA PA Program is 27 months in length, consisting of 15 months (4 semesters) of didactic training and 12 months (3 semesters) of clinical training. Graduates must successfully complete all aspects of the PA program, which must be accredited by the ARC-PA, and pass the Physician Assistant National Certifying Examination (PANCE) in order to obtain a license in the state(s) in which they desire to practice. Upon graduation, graduates will have the ability to practice in any of the different specialties of medicine. Licensed and certified PAs are required to complete 100 hours of continuing medical education every two years and pass the required NCCPA certification requirement every ten years in order to maintain certification.
Candidates for admission must meet the following requirements:
Please note that the CUAA PA program will review transcripts for repeated courses and withdrawals. The presence of multiple repeats and/or withdrawals will be taken into consideration when deciding progression through the admissions process and acceptance into the program.
The program will specifically use the grades from CUAA science pre-requisites delineated (including repeats and withdrawals) to create a calculated GPA in CASPA for only those science courses that are required by the program. This may create a discrepancy between the calculated CUAA prerequisite science GPA and the CASPA "global" science GPA of all science courses taken.
All science prerequisite courses must be completed within 8 years of the time of application and must be completed with a C grade or better. All science prerequisite coursework must be completed at the time of application in CASPA. Applications with missing science prerequisites will not be considered.
* If specific AP courses are not listed on college transcript, please send official AP score transcript to gradpa@cuaa.edu
The Concordia University Ann Arbor PA Program is recommending their applicants take the PA-CAT (Physician Assistant College Admission Test). The PA-CAT is a specialized test designed to measure applicant knowledge in key prerequisite science subjects typically required for PA school. For information about the PA-CAT and to schedule your exam click here.
PA-CAT Study materials provided by Exam Master include:
PA-CAT Covered Subjects: Anatomy, Physiology, General Biology, Biochemistry, General and Organic Chemistry, Microbiology, Behavioral Sciences, Genetics, Statistics.
The CUAA PA program has specific academic and technical standards that apply to all candidates for admission and those selected to enter the program.
Students must attest that they meet these standards prior to matriculation, and must continue to meet these standards for the entire duration of the program in order to complete the curriculum and to achieve the Master of Science in Physician Assistant Studies degree.
Accommodation may be possible for some disabilities, but the Physician Assistant’s role in providing healthcare requires the ability to perform all the duties independently without compromising patient care.
To perform the functions required of a Physician Assistant in various clinical settings and deliver competent patient care, as stipulated by the faculty, accreditation agencies, and PA practice standards, all candidates/students for the program must independently meet the following Academic and Technical Standards. Candidates/students are prohibited from using aid from trained intermediaries.
The PA program at Concordia University Ann Arbor retains the authority and responsibility for the selection and evaluation of students. Admitted candidates will be required to certify in writing that they understand and meet the academic and technical standards of the program. Accommodations for disabilities may be available and will be evaluated on a case-by-case basis. Concordia University will make every effort to develop mechanisms to accommodate otherwise qualified candidates; however, the integrity of the curriculum and the need to provide optimal patient care must be preserved to ensure that all aspects of PA education are effectively delivered to all students.
Observational Standards
PA students must have sufficient sensory capacity to independently observe in lecture halls, laboratories, outpatient settings, and at the patient’s bedside. Required sensory skills include functional vision, hearing, olfaction, and tactile sensation. These skills must be adequate to observe a patient’s condition and gather information through common physical examination procedures such as inspection, auscultation, percussion, and palpation.
Communication Standards
PA students must communicate effectively and efficiently with all individuals they encounter, including patients, their families, healthcare workers, faculty, staff, and classmates. Students must be able to obtain medical histories promptly, interpret non-verbal communication, and establish professional relationships with patients. Additionally, students must accurately and clearly record information and present data in a concise and logical manner.
Motor Standards
PA students must have the endurance to tolerate physically demanding workloads and be able to transport themselves promptly from one location to another. After a reasonable training period, students must independently perform physical examinations and diagnostic maneuvers, such as palpation, auscultation, percussion, and other diagnostic techniques. Students must be able to respond promptly to clinical problems and provide direct general and emergency treatment to patients in various circumstances. Examples include, but are not limited to, cardiopulmonary resuscitation, the administration of intravenous medication, the application of pressure to stop bleeding, the opening of obstructed airways, the suturing of simple wounds, and the performance of basic obstetrical maneuvers. These activities require physical mobility, gross and fine neuromuscular coordination, and equilibrium. Additionally, students must adhere to safety standards appropriate for clinical settings and follow universal precautions, including wearing complete sets of Personal Protective Equipment (PPE) for extended hours.
Conceptual, Integrative, and Quantitative Standards
Students must be able to assimilate and engage with detailed and complex information presented through both the didactic and clinical curriculum. They are expected to estimate, measure, calculate, analyze, synthesize, and outline information quickly and efficiently. Additionally, students must comprehend three-dimensional and spatial relationships of structures, interpret connections, and make accurate, fact-based conclusions based on the patient’s history, clinical presentation, physical examination results, and laboratory studies. They must also adapt to various learning environments and effectively learn, participate, collaborate, and contribute as part of a team.
Behavioral, Social, and Professional Standards
Students must exhibit sufficient maturity and emotional stability to fully utilize their intellectual abilities. This includes exercising good judgment and promptly completing all responsibilities associated with patient diagnosis and care. Understanding the legal and ethical aspects of medical practice and functioning within these standards is essential. Students must demonstrate integrity, honesty, professionalism, and compassion, and show a spirit of cooperation and teamwork at all times.
Students are expected to interact courteously, professionally, and respectfully with patients, their families, healthcare professionals, colleagues, faculty, and staff. They should demonstrate empathy and compassion for all patients while accommodating varying levels of health literacy. Additionally, students must take responsibility for their learning and implement positive changes in response to constructive feedback.
Students must also demonstrate the physical and emotional endurance necessary to handle demanding workloads. They should perform competently and professionally in high-stress, fast-paced situations, adapt to changing environments, display flexibility, and manage the inherent uncertainties of patient care and the healthcare system.
Class of 2027
Class of 2028
Applicants who do not successfully complete their Bachelor’s degree prior to the first day of class, will not be allowed to matriculate into the program.
Many of the health care organizations that we partner with for our clinical rotations require a criminal background check for student participation. By applying, applicants understand that placement at these clinical sites, required for the Concordia University Ann Arbor Physician Assistant program, may be affected by the results of a criminal background check.
All students accepted into the PA program will be required to complete and pass a background check. A felony conviction will impact our admission decision.
It has been the program’s experience that those students who choose to work after admission to the program are most often unable to complete the program successfully. For this reason, the program strongly recommends that students NOT work for the duration of the PA program. Working outside of the PA program will not be given consideration in evaluating a student who fails to meet program requirements.
As a matter of policy, Concordia University admits students of any age, race, color, gender, religion, and national and ethnic origin. Admitted students enjoy the rights, privileges, programs and activities generally offered to all Concordia students. Further, Concordia University does not discriminate according to age, race, color, gender, and national and ethnic origin in administering admissions and educational policies, scholarship and loan programs, and athletic and other school-administered programs.
Accommodations for Students with Disabilities: Concordia University is committed to full compliance with the Americans With Disabilities Act of 1990 (ADA) and Section 504 of the Rehabilitation Act of 1973, which prohibit discrimination against qualified persons with disabilities, as well as other federal and state laws pertaining to individuals with disabilities. Under the ADA and its amendments, a person has a disability if he or she has a physical or mental impairment that substantially limits a major life activity. The ADA also protects individuals who have a record of a substantially limiting impairment or who are regarded as disabled by the institution whether qualified or not. A substantial impairment is one that significantly limits or restricts a major life activity such as hearing, seeing, speaking, breathing, performing manual tasks, walking, or caring for oneself.
Concordia University is committed to providing qualified students with disabilities with reasonable accommodations and support needed to ensure equal access to the programs and activities of the University.
All accommodations are made on a case-by-case basis. A student requesting any accommodation should first contact the Director of Disability Services who coordinates services for students with disabilities. The director reviews documentation provided by the student and in consultation with the student, determines which accommodations are appropriate to the student’s particular needs and programs. It is then the student’s responsibility to make direct requests for accommodations to the appropriate staff.
As a potential candidate, the admissions committee will look at the following for acceptance into the program:
A holistic overview of the applicant is performed by all reviewers who will score applicants based on the following criteria:
CU graduates and alumni will be granted an automatic interview with successful completion of all requirements AND a 3.0 GPA in BOTH cumulative AND pre-requisite coursework
Applicants who are military veterans, and have a minimum 3.0 GPA in BOTH cumulative AND pre-requisite coursework, will be granted an automatic interview with successful completion of all requirements.
In upholding our mission and vision, if there are two equally qualified candidates with similar GPAs, coursework, letters of recommendation, and patient care experience, the applicant who provides service to others in community or church would be selected over the one who does not serve.
In upholding our program's mission, in making a selection between equally qualified candidates, candidates from HPSA (health professional shortage areas), rural communities, and MUC (medically underserved communities) will be given preference. This is in fitting with the mission and vision of the PA program. To check qualification use the links below:
Similarly, when selecting between equally qualified candidates, those who are first generation college students or low income students will be given a preference with successful completion of all admission requirements.
Concordia University Ann Arbor’s Master of Science in Physician Assistant Studies program has received the maximum 10-year accreditation from the ARC-PA—an exceptional affirmation of program quality, student preparation, and faculty excellence. Read the full story.
The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) has granted Accreditation-Continued status to the Concordia University – Ann Arbor Physician Assistant Program sponsored by Concordia University – Ann Arbor. Accreditation-Continued is an accreditation status granted when a currently accredited program is in compliance with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be July 2035. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.
The program’s accreditation history can be viewed on the ARC-PA website.
The Concordia University Ann Arbor MSPAS program will publish first time Physician Assistant National Certifying Exam (PANCE) rates for the five most recent graduating classes as provided by the National Commission on Certification of Physician Assistants (NCCPA). Please visit this link to review our program's NCCPA Exam Performance Summary Report.
Please note that thus far, the program has had two graduating cohorts. The class of 2025 will graduate in December of 2025. The class of 2026 will graduate in December of 2026. PANCE scores for these cohorts will be posted once all students have taken their exam, typically 3-6 months after graduation.
| Class | Class Graduation Year | Group | Number of Candidates Who Took PANCE | Number of Exam Attempts | Number of Exams Passed | Program Exam Pass Rate | National Exam Pass Rate for the Class Graduation Year | % of Candidates Who Ultimately Passed PANCE |
|---|---|---|---|---|---|---|---|---|
| Class of 2023 | 2023 | All Takers | 30 | 33 | 30 | 91% | 89% | 100% |
| First Time Takers | 30 | 30 | 28 | 93% | 92% | 100% | ||
| Class of 2024 | 2024 | All Takers | 31 | 32 | 30 | 94% | 89% | 97% |
| First Time Takers | 31 | 31 | 29 | 94% | 92% | 97% |
Graduated classes |
||||
| Class of 2023 | Class of 2024 | Class of 2025 | Class of 2026 | |
|---|---|---|---|---|
| Maximum entering class size (as approved by ARC-PA) |
32 | 40 | 40 | 40 |
| Entering class size | 32 | 35 | 38 | 35 |
| Graduates | 30 | 31 | # | # |
| * Attrition rate | 6% | 11% | 3% | 6% |
| **Graduation rate | 94% | 89% | # | # |
*Attrition rate calculation: number of students who attritted from cohort divided by the entering class size.
**Graduation rate: number of cohort graduates divided by the entering class size.
Class of 2023
Class of 2024
Class of 2025
Class of 2026
At the completion of the PA program, students will:
This goal aligns with our mission statement, which is “to educate Physician Assistant students in primary medicine with a focus on rural and underserved patient populations and communities.” Our program utilizes applicant self-reported designations through CASPA regarding rural and medically underserved status identifier and additionally confirmed by verification permanent addresses utilizing Rural Health Grants Eligibility Analyzer to identify candidates from the applicant pool that meet this criterion. The program was awarded a HRSA grant, which aids in fulfilling its mission of matriculating applicants from these rural* and medically underserved areas** into the program.
* Rural: The United States Census Bureau and Office of Management and Budget (OMB) does not define “rural.” They consider “rural” to include all people, housing, and territory that are not within an urban area. Any area that is not urban is rural. (Health Resources & Services Administration: Defining Rural Population, April 16, 2024)
** MUA: Medically underserved area = a shortage of primary health care services for residents within a geographic area as designated by HRSA. (U.S. Dept. of Health & Human Services Guidance Portal: Types of Designations, April 16, 2024)
| Criteria | Class of 2023 | Class of 2024 | Class of 2025 | Class of 2026 |
|---|---|---|---|---|
| Number of students matriculated per cohort | 32 | 35 | 38 | 35 |
| Matriculation (Rural* and/or MUA**) |
18 Students, 56% |
17 Students, 48% |
16 Students, 42% |
12 Students, 34% |
| Graduation (Rural* and/or MUA**) |
100% (May, 2023) | 94% (May, 2024) | TBD (December, 2025) | TBD (December, 2026) |
The goal of this initiative is to expose students to the unique challenges and rewards of practicing in underserved and underrepresented communities. The HRSA grant allows the program to provide students with monetary stipends in HRSA qualified areas and qualified rural health care clinics to increase clinical learning opportunities. PA students engage with PAs practicing in rural settings who share their insights and experiences through lectures. By experiencing firsthand the critical need for healthcare professionals in these areas, we hope to cultivate a greater interest among students in pursuing careers in such settings after graduation.
| Criteria | Class of 2023 | Class of 2024 | Class of 2025 | Class of 2026 |
|---|---|---|---|---|
| Number Of Students | 30 | 31 | 37 | 35 |
| Percentage of students performing a clinical rotation in a rural and/or medically underserved area | 46% (May, 2023) | 64% (May, 2024) | TBD (December, 2025) | TBD (December, 2026) |
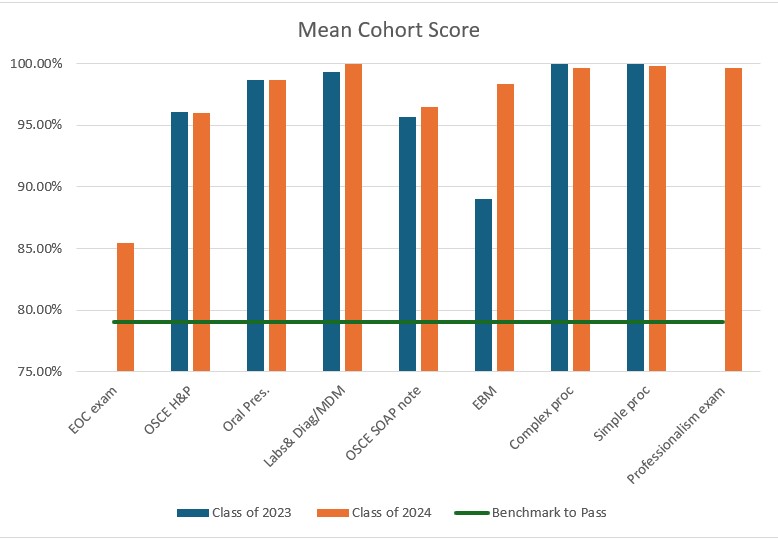
The program is focused on primary care medicine as indicated by our program competencies. As such, our students are evaluated for their preparedness for entry level clinical practice with the Program Summative Assessment (which includes the End of Curriculum Exam), Student Exit Survey, End of Curriculum Survey, Preceptor Evaluation of Student, Student End of Didactic Terms Survey, and the PANCE certification.
| Assessment Tool | Assessment Question | Class of 2023 Mean Score |
Class of 2024 1 Mean Score |
|---|---|---|---|
| Preceptor Evaluation of Student | |||
| 5-Point Preceptor Scale 2 | To what extent was the student prepared for this rotation? | 4.64 | 4.84 |
| Total amount of evaluations | 270 | 248 | |
| Student Exit Survey | |||
| 5-Point Program Survey Scale 3 | Rate your satisfaction with each of the following statements regarding how your clinical education prepared you for entry level practice in primary medicine: clinical intervention for patient presentations | 4.40 | 4.52 |
| 5-Point Program Survey Scale 3 | Rate your satisfaction with each of the following statements regarding how your clinical education prepared you for entry level practice in primary medicine: ability to effectively function in an inter-professional healthcare team | 4.45 | 4.62 |
| 5-Point Program Survey Scale 3 | Rate your satisfaction with each of the following statements regarding how your clinical education prepared you for entry level practice in primary medicine: ability to create a management plan for the patient | 4.35 | 4.55 |
| Total amount of students who completed an evaluation | 20 | 29 | |
| Student End of Didactic Terms Survey | |||
| 5-Point Program Survey Scale 3 | I feel adequately prepared for clinical rotations following the didactic coursework in the following areas: clinical intervention for patient presentations | N/A 4 | 4.50 |
| 5-Point Program Survey Scale 3 | I feel adequately prepared for clinical rotations following the didactic coursework in the following areas: ability to effectively function in an inter-professional healthcare team | N/A 4 | 4.60 |
| 5-Point Program Survey Scale 3 | I feel adequately prepared for clinical rotations following the didactic coursework in the following areas: ability to create a management plan for the patient | N/A 4 | 4.50 |
| Total amount of students who completed an evaluation | N/A 4 | 20 | |
1Class of 2025 will complete End of Didactic Survey in December 2024.
2Preceptor scale is Excellent (5), Good (4), Average (3), Below average (2), Poor (1).
3Program survey scale is Strongly agree (5), Agree (4), Neither agree nor disagree (3), Disagree (2), Strongly disagree (1).
4Questions were not on the end of didactic term survey for the class of 2023.
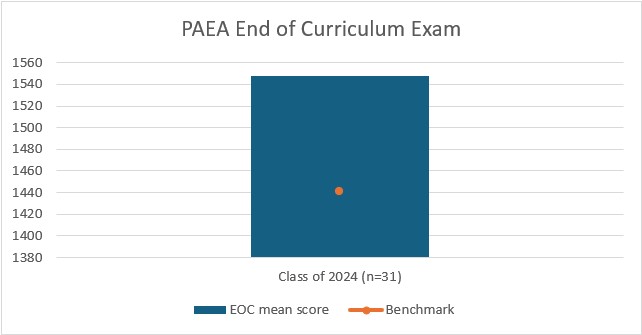
The PAEA threshold for satisfactory performance is 1400. CUAA's overall mean score is 1547.58 (low of 1432)
ꭞClass of 2023 had CUAA designed EOC
| Class of 2023 | Class of 2024 | |
|---|---|---|
| Number of Students | 30 | 31 |
| EOC exam | N/A | 100% |
| OSCE H&P | 100% | 100% |
| Oral Pres. | 100% | 100% |
| Labs & Diag/MDM | 100% | 100% |
| OSCE SOAP note | 100% | 100% |
| EBM | 100% | 100% |
| Complex proc- EKG | 100% | 100% |
| Simple proc- Vitals | 100% | 100% |
| Professionalism exam | N/A | 100% |
Assistant Professor
Office: Ann Arbor North Building 306
Phone: (734) 995-7318
Experienced PA with 10+ years in clinical practice, with recent transition into academia. Passionate about teaching and simplifying complex medical concepts a clear and concise manner.

Assistant Professor
Office: Ann Arbor North Building 340

Assistant Professor
Hi, I’m Dr. LaKreese Johnson. I’ve been a physician assistant for over 16 years, and even before that—five years prior—I was a passionate patient advocate, which ultimately led me back to school to pursue my PA career path. With a Doctor of Medicine, a Master’s in Physician Assistant studies, and a Bachelor of Science in Psychology, I’ve built my career on combining clinical expertise with genuine compassion for the patients I serve. When I’m not caring for patients, you can find me traveling, skating, or soaking up the peace of nature—experiences that keep me grounded and continually inspired in my work.

Assistant Professor
Office: Ann Arbor North Building 308
Phone: (734) 995-7445
I graduated from Central Michigan University PA Program in 2020 and my clinical experience thus far has been in Internal Medicine, primarily Hospital Medicine. I am passionate about sharing my experiences and knowledge with the next generation of physician assistants.

Program Director - Physician Assistant Studies at CUAA, Assistant Professor
Office: Health Services 308
Phone: (734) 995-7489
I have been a licensed PA for 32 years in the specialty of Emergency Medicine. My degrees are BS PA from WMU, MS PA from Univ. of Nebraska, Lincoln and a DMSc from Lynchburg University. I teach Skills, Patient Care, and Emergency Medicine.

Associate Professor
Office: Ann Arbor North Building 305
Phone: (734) 995-7492
Dr. Shuman-Donnelly joined the faculty of CUAA in August 2017. She is currently an Associate Professor of Physician Assistant Studies and Physical Therapy teaching Anatomy and Physiology for the School of Health Professions (May 2025-present). Prior to this appointment, she ran the undergraduate Exercise Science program (BS) and the implementation of the programs curriculum from 2017-2025. Prior to CUAA, Dr. Shuman-Donnelly was the Director of Strength and Conditioning at Idaho State University, where she designed, implemented, tested, and evaluated over 300 student-athletes. Her experience in the weight room, as well as the copious amount of time spent performing research in the Human Performance Lab translated directly into the classroom. A Registered Strength and Conditioning Coach (RSCC), a well deserved recognition, as well as a Certified Strength and Conditioning Specialist (CSCS), both through the National Strength and Conditioning Association, makes Dr. Shuman the resident expert on sport performance and injury prevention.

Assistant Director - Clinical Education, Assistant Professor
Office: Ann Arbor North Building 315
Phone: (734) 995-7381

- Medical Director - Physician Assistant Studies

Director of Clinical Education - Physician Assistant Studies - CUAA, Clinical Assistant Professor
Office: Ann Arbor North Building 314
Phone: (734) 995-7306
I am passionate about sharing my clinical experience with the next generation of Physician Assistants and showing Christ's love where He places me to serve.

(fees are subject to change)
| Matriculation Date: | August 2025 | August 2026 |
| Total PA Tuition: Paid in five installments |
$99,600 | $102,500 |
| Fees*: Includes Graduation Fee, Technology Fee, University Lab Fee, and Student Services; paid per Fall and Spring semester |
$593 | $615 |
| Parking: Paid once per year (Didactic) |
$200 | $200 |
Total tuition for the entire PA Program is listed above. You will be billed in five installments (once each Fall and Spring Semester).
*Costs are the same for both resident and non-resident. Student’s own food, transportation and housing costs are not included.
Please note: costs will vary depending on the equipment selected by the student
| Items | Student Costs |
| Books | ~$450 books in print Most texts available online through AccessMedicine |
| Laptop**** | ~ $600-1200 |
| Medical Equipment | ~$900-1200 (Students do not need to buy equipment they already have) |
| EXXAT | ~$450.00 |
Student housing may be required at clinical sites; all housing and transportation costs are the responsibility of the student.
Students who withdraw from the University will receive a pro-rated refund of educational fees and board fees, according to the following schedule (a week runs Mon-Sun):
| DURING FIRST WEEK OF CLASSES | 80% |
| DURING SECOND WEEK OF CLASSES | 75% |
| DURING THIRD WEEK OF CLASSES | 60% |
| DURING FOURTH WEEK OF CLASSES | 40% |
| DURING FIFTH WEEK OF CLASSES | 20% |
| AFTER FIFTH WEEK | none |
Students who are charged for summer term but then withdraw will receive refunds on a pro-rated basis as follows:
| DURING FIRST DAY OF CLASS | 80% |
| DURING SECOND DAY OF CLASS | 75% |
| DURING THIRD DAY OF CLASS | 60% |
| DURING FOURTH DAY OF CLASS | 40% |
| DURING FIFTH DAY OF CLASS | 20% |
| AFTER FIFTH DAY OF CLASS | none |
Your generous contribution of time, hard work and medical expertise on the part of our students is the vital key to the success of the CUAA PA program and to the success of our students when they graduate.
The clinical experiences the student will obtain under your supervision are critical in synthesizing the concepts and application of principles for high quality health care delivery. Twelve months of clinical rotations follow fifteen months of rigorous didactic coursework. You, the preceptor, are vital to successful learning in the clinical setting. The PA student will work closely with you, and s/he will progressively develop the skills and clinical judgement necessary to become a practicing PA. Thank you for your commitment to PA education!
Following is the link to the clinical preceptor handbook which highlights policies and procedures:
Students who continue to work find that they struggle to find the time to review material. Students need the evenings and weekends to review course material, complete assignments, and read new material. While the program does not forbid working in the program, it is important to note that students that do find it impacts their grades and ability to successfully complete the program.
As you consider a career in healthcare, it is important to know that due to the nature of training of Physician Assistant Students there is the potential of exposure to infectious or environmental contacts that may lead to disease or disability. The Program provides education on Universal Precautions and how to protect yourself both as a student and healthcare provider with in-class education, online modules and tests; and reminders throughout the program length about best practices.
The PA program follows the Centers for Disease Control and Prevention (CDC) guidelines for healthcare personnel on immunization. Students are responsible for any financial costs related to immunization and screening requirements. The PA program requires the following immunizations:
*NOTE: While CUWAA does not require vaccinations, many of the universities' clinical partners require that students who learn in their facilities are vaccinated against specific communicable diseases. Such policies are developed and administered by the clinical partners, and those facilities may, in some cases, grant exemptions to their own vaccine requirements. However, on the advice of legal counsel, CUWAA does not review or grant exemptions/waivers/exceptions to policies developed by other entities. Students who choose to enroll in a CUWAA health care program must adhere to all vaccine requirements of the clinical facilities to which they are assigned. Further, CUWAA is not obligated to reassign students to a different clinical experience or facility based on vaccination status, or for any other reason. An employer exemption (from an organization you are employed by, for example) does not carry over to the CUWAA student role. Once a decision on the student exemption has been made by the organization, the approval form or email needs to be forwarded to the staff member that handles your onboarding process.
CUAA is committed to equality of opportunity and does not discriminate against applicants, students, or employees based on race, religion, color, national origin, gender, age, sexual orientation or disability. CUAA PA students have equal access to facilities and programs of the Concordia University Ann Arbor as any student from any of the other programs.
Attendance is MANDATORY for all lectures and labs. The program will give you advance notice for evening and weekend labs/requirements.
The student must contact the Program Director or course director for the class(es) that they will miss.
The following are considered excused absences, but must be reported to the course director and Program director by email or in person in advance if at all possible.
Students must schedule their medical appointments outside of class or rotation time.
Appointments may be kept without incurring an unexcused absence if that appointment was made, and the course time schedule was changed and student was unable change their medical appointment on short notice.
Anything other than #’s 1-5 above will be considered an unexcused absence.
If a second unexcused absence occurs, the student will appear before the Student Progress Committee. No credit or make up will be given for missed assignments, quizzes, exams, or labs. Any student excused from a class is responsible for obtaining the missed material. If the absence is expected to go beyond 3 days, the student must contact the Program Director and a note from the student’s provider will be needed to return to class. Make up class or lab assignments are provided solely at the discretion of the course director. Multiple excused absences may be brought before the Student Progress Committee.
Students are responsible for being in their seat in the classroom prior to the start of lecture. The tardy student will be responsible for any missed content. Repeated tardiness or absences are inconsistent with the professional expectations noted in the handbook. The AA will notify the PD when there is a tardy form turned in by faculty. Tardiness is not acceptable and is a professionalism infraction and may be referred for additional sanctions (see handbook for more detail).
Please Note: Details about the requirements for the successful completion of the didactic year can be found in the Student Didactic Handbook section titled "Requirements for Completion of Didactic Year."
In addition to these academic requirements, the student must also:
The program will monitor student progress in a timely and ongoing fashion, and will provide remediation options for the student to improve performance. It is the student’s responsibility to make significant efforts at remediation to prove competency. Processes for remediation are outlined in both the Didactic and the Clinical Student Handbook.
In accordance with Std. A3.03, it is the responsibility of the Program to solicit and provide clinical sites and preceptors, not the student’s responsibility. Prospective and enrolled students will not be asked to solicit sites, recommend preceptors, nor be required to find their own clinical sites. Contact the Director of Clinical Education for appropriate process to follow should you have a site or preceptor that you may want the program to consider.
Please Note: Details about the requirements for the successful completion of the clinical year can be found in the Student Clinical Handbook section titled "Academic Progression."
In addition to these academic requirements, the student must also:
The CUAA’s PA Program reserves the right to dismiss any PA student at any time prior to graduation. Circumstances warranting such action may be of an academic, legal or professional nature. Additional information is available in the student handbooks on appeal of dismissal and withdrawal from the program.
The student handbooks (both didactic and clinical) are available as a link in the accreditation tab on this website for additional review of program policies.
The CUAA PA program does not decelerate students for failing to meet the program’s academic and/or professionalism requirements.
Students may request a temporary stop-out in writing to the Program Director, and will be required to provide written evidence of the medical issue related to the request. Prior to the student’s return to the program, the Program Director will provide the student with a specific deceleration plan. This plan will be developed on a case-by-case basis after review and with input from the student’s advisor, the Student Progress Committee and the Program Director.